Periodontitis
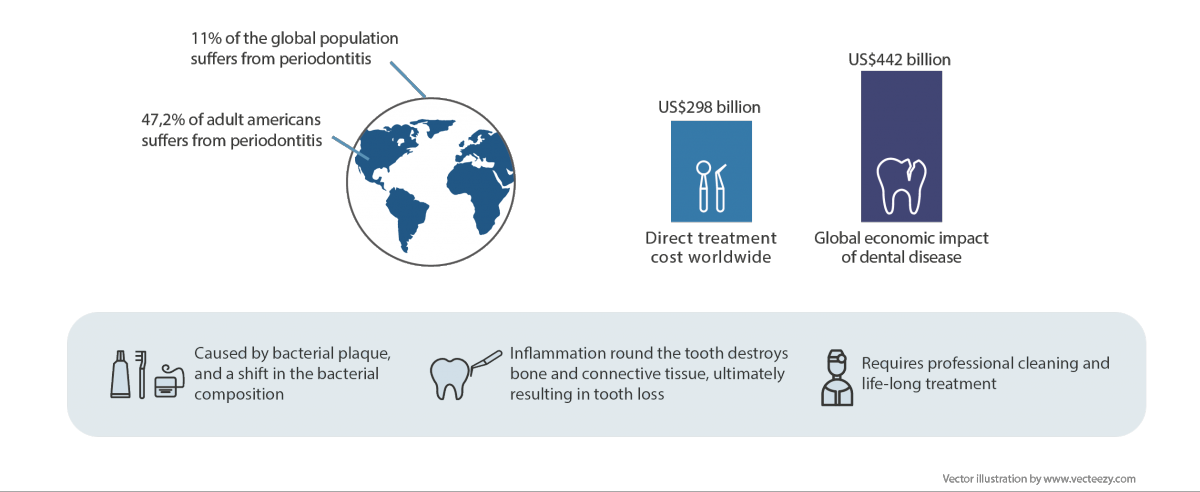
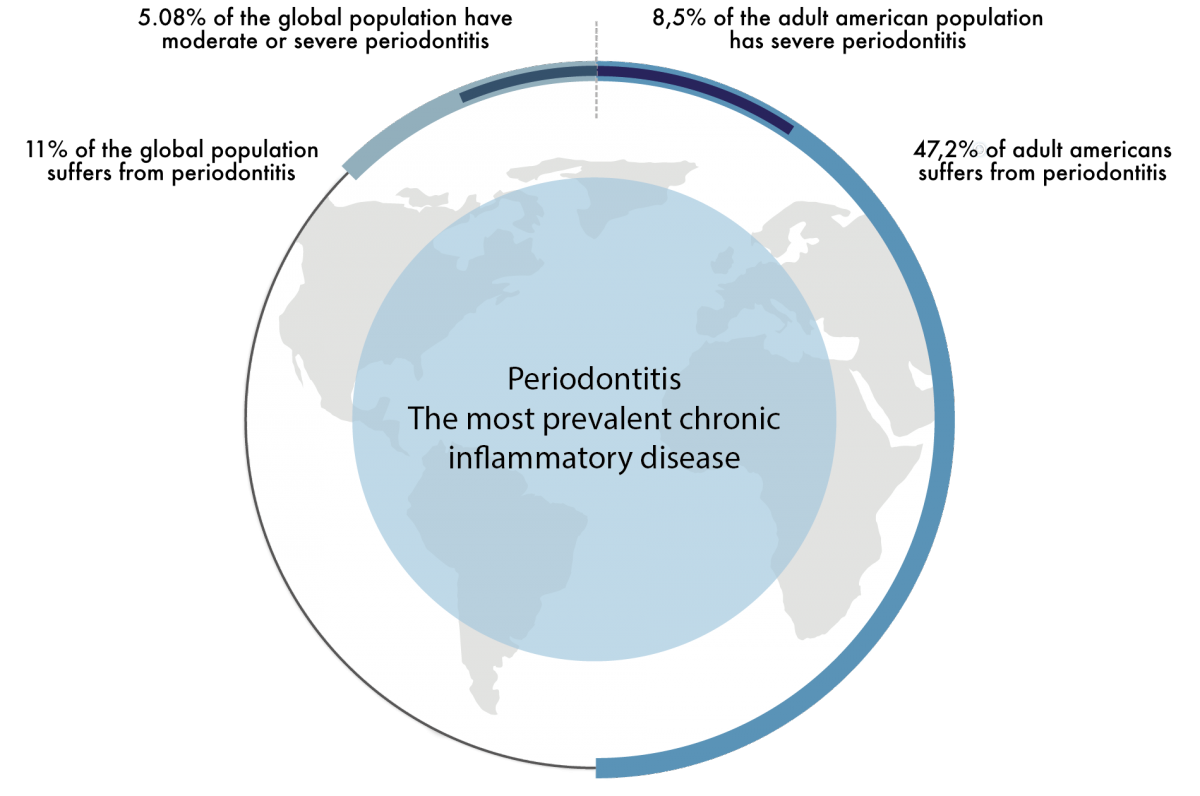
With cancer and stroke taking center stage as leading causes of death in industrialized nations, periodontitis, the most prevalent chronic inflammatory disease induced by bacteria, remains a clearly underestimated health problem.
Approximately 9% of people are losing teeth due to severe periodontitis, a fact that sadly in many societies still is accepted as a natural consequence of ageing.
Even more alarming however, is the mounting evidence that points to causative relationships between periodontitis and diseases such as rheumatoid arthritis, chronic obstructive pulmonary disease, cardiovascular disease, diabetes mellitus and various types of cancer. Thus, taking into account the direct impact of periodontitis on public health as well as its negative associations with an array of debilitating and life threatening diseases, it is unquestionable that this disease represents an immense and unmet medical challenge.
It is now the general consensus that a small consortium of bacteria, termed the “red complex” and comprising P. gingivalis, T. denticola and T. forsythia, orchestrates the pathological changes in the periodontium manifested as periodontitis. By invading the microbial community that populates a tooth’s surface, these bacteria trigger shifts in the composition of this dental biofilm leading to the development of periodontitis. P. gingivalis is considered the “keystone” pathogen, due to its unsurpassed capacity to initiate an individual’s transition from having a commensal oral microbiome to a state of pathogenic microbial imbalance. Thereof, elimination of P. gingivalis is pivotal in treatment and prevention of periodontitis.